A pass-through billing scheme is an improper practice for reference-laboratory billing when a healthcare provider pays a lab for a test but files the claim to have done the test themselves. While it may seem like a simple way to expand services, it can quickly become a legal nightmare for hospitals and physician offices.
This guide will help you understand everything you need about pass-through billing for labs, from the potential liability risks to proper billing compliance for extremely limited exceptions.
Please refer to CMS’s Examining Clinical Laboratory Services and Chapter 16 of the Medicare Claims Processing Manual to understand the technicalities. Or contact us for lab-specific billing services to help you avoid pass-through billing pitfalls.
What is Pass-Through Billing for Labs?
Pass-through billing in labs is a scheme where a healthcare provider such as a hospital or a practice bills a patient or insurance company for lab tests, even though a different lab performs those tests.
An example of a pass-through billing scheme would be a provider offering specialized medical services, such as genetic testing, that needs to be adequately reimbursed. The government payer or private insurer would provide pass-through payments to cover the additional costs for the associated services.
Why Pass-Through Billing Scheme
Providers or laboratories would go for pass-through billing for many reasons.
- Sometimes, a lab has no contractual relationship with an insurance company. Pass-through billing for labs allows the provider, who likely has such a contract, to act as a middleman and bypass this hurdle.
- A lab with questionable practices might use a provider as a shield to avoid direct scrutiny from payers.
- Providers might see pass-through billing as a way to get financial benefits associated with in-office testing without the costs of operating their lab.
Here’s how pass-through billing works:

1. Lab-to-Lab Pass-Through Billing Arrangements
An independent or hospital lab might send a test they can’t perform themself to a specialized “reference lab” for analysis. However, the original lab would then bill the patient or insurance for the test, not the reference lab that actually conducted it. This is exactly what is called the “Pass Through Billing for Labs.”
2. Provider-to-Lab Pass-Through Billing Arrangements
Similar to the lab-to-lab scenario, a physician may draw blood or collect a sample and send it to an outside lab for testing. The physician’s office then bills the insurance or patient for the test, even though their in-house lab didn’t perform it.
These are two significant pass-through billing arrangements, but it’s important to distinguish them from legitimate reference lab billing practices.
What is Not a Pass-Through Billing Scheme
Legit reference lab billing practices are not part of a pass-through billing scheme. And it has two major scenarios.
a) Focus on Pass-through Billing
Pass-through billing primarily focuses on the billing aspect, not necessarily the location where the test is performed. So, a reference lab might conduct the test, and the lab or physician’s office should only submit the claim if they themselves performed the test.
b) Reference Labs in Pass-Through Billing
In a legitimate scenario, the reference lab would bill the original lab (which then bills the patient or insurance) with precise and actual documentation. However, in a pass-through billing scheme, providers or labs bypass the reference lab entirely in terms of billing, creating a fraudulent situation.
Why Avoid Pass-Through Billing Scheme
There are many problems with pass-through billing for labs, such as double billing to payer companies, inflated charges or unnecessary tests, compromised test quality, and violation of laws. Let us explain these issues associated with the billing scheme.
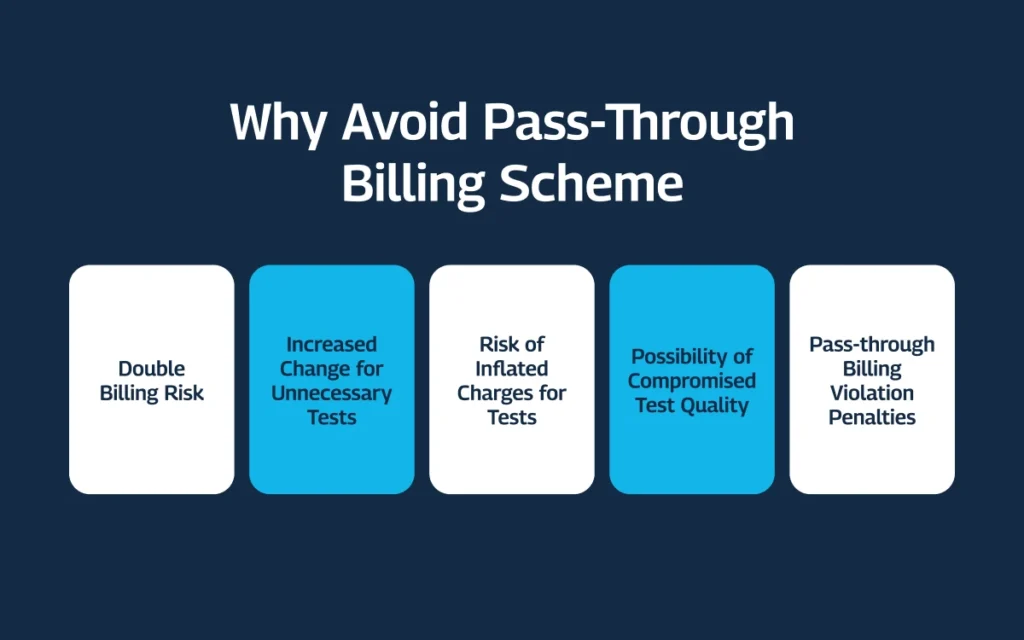
1. Double Billing Risk
The provider (who didn’t perform the test) and the actual testing lab could submit claims for the same test, leading to double billing for insurance companies.
2. Potential for Abuse
Pass-through billing for labs can cause inflated charges or unnecessary tests. The provider billing for the test might exceed the cost compared to what they paid for the actual testing lab, leading to unfair billing practices.
3. Compromised Test Quality
Delays in sending samples or improper handling by the intermediary provider or laboratory could affect the test results’ accuracy.
4. Pass-through Billing Violations Are Illegal
In most cases, pass-through billing for labs is illegal and a violation of multiple federal healthcare fraud and abuse laws, such as the Anti-Kickback Statute (AKS), False Claims Act (FCA), and Stark Law.
The consequences for violating these laws can be severe, including significant fines, penalties, and even exclusion from federal healthcare programs. And it can also lead to significant reputational damage for labs and healthcare providers.
4.1 Anti-Kickback Statute (AKS)
This law prohibits kickbacks or financial incentives for referrals for services covered by Medicare or Medicaid. A lab marking up the cost of a test performed by another lab could be a kickback to the provider for sending the test their way.
4.2 False Claims Act (FCA)
Submitting false claims to government payers (like Medicare or Medicaid) for services not rendered is a pass-through billing violation of this act. Since the provider didn’t perform the test, billing for it would be considered a false claim.
4.3 Physician Self-Referral Law (Stark Law)
Stark Law prohibits doctors from referring patients for certain services to entities with which they (or an immediate family member) have a financial relationship. Pass-through billing often involves such a financial connection and thus is considered illegal.
These are just the three primary violations of pass-through billing for labs. Depending on the specific situation, other laws might be applied as well. Also, many states prohibit pass-through billing and mandate direct billing as the only acceptable practice.
Note: Labs and healthcare providers must prioritize proper billing practices and explore alternative solutions, such as establishing legitimate reference lab relationships or considering in-house testing capabilities.
Limited Exceptions to Pass-Through Billing for Labs
While pass-through billing is generally illegal, and some people even call it a scam, there are a few exceptions, primarily for Medicare. But you must still be extremely careful when approaching these exceptions, ensuring compliance with all the regulations.
Rural Hospitals
In some cases, rural hospitals with limited laboratory services can use pass-through billing for specific tests they cannot perform. But again, you must stay compliant with proper documentation and guidelines.
Common Ownership
Pass-through billing for labs might be allowed if the billing and testing labs have common ownership; for example, both are part of the same hospital system. Also, under certain conditions, you must verify eligibility with Medicare and ensure you follow the best billing practices.
Limited Referrals
In some cases, physicians can refer a patient to a specific lab for a limited number of tests if they do the proper documentation and adhere to Stark Law regulations. However, you cannot use this exception to pass-through billing for most scenarios, and you must also consider its legal implications.
These exceptions primarily apply to Medicare. Commercial insurance companies and state Medicaid programs may have different policies for pass-through billing for labs and physicians.
Note: Laboratories must always verify eligibility with each payer (Medicare, commercial insurance, and state Medicaid) before considering any pass-through billing to avoid potential issues with claim denials or accusations of fraud.
Proper Billing Procedures (For the Exceptions)
Even in the limited exception scenarios, you must apply proper billing procedures to ensure compliance.
1. Use Modifier 90
When billing for a test performed by another lab under an exception, you must use modifier 90 on the claim form. The modifier identifies the test as referred to another lab.
2. Separate Claims for In-House & Reference Lab Tests
If a lab performs some tests in-house and refers others to a reference lab under an exception, you must submit separate claims for each set of tests, often done on paper.
3. Maintain CLIA Certification
Labs can only bill for tests for which they hold the appropriate Clinical Laboratory Improvement Amendments (CLIA) certification. This applies even if a reference lab performs the test under an exception. The billing lab is responsible for the test quality.
Note: Legalities of pass-through billing for labs and physician offices, even with exceptions, are complex. Consulting with lab billing services, a qualified medical billing consultant for labs, ensures compliance and helps avoid legal and financial consequences.
How to Avoid Pass-Through Billing for Labs
Pass-through billing for labs and physicians can be a tempting shortcut, but the risks outweigh the potential benefits. Here’s how labs can avoid the pitfalls and ensure compliance with proper billing practices:
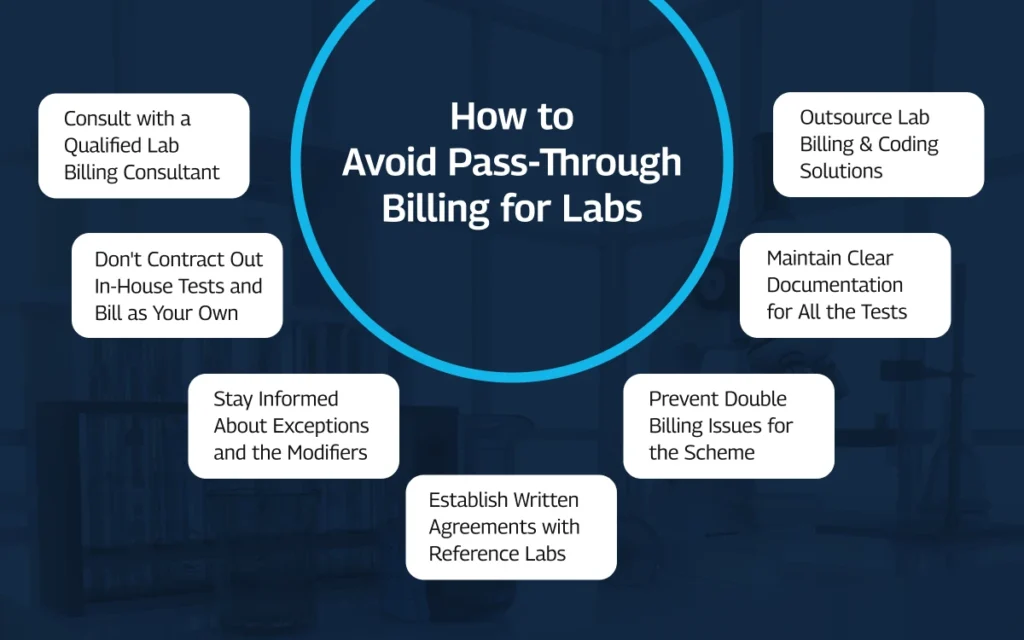
- Consult with a Qualified Lab Billing Consultant
- Don’t Contract Out In-House Tests and Bill as Your Own
- Stay Informed About Exceptions
- Establish Written Agreements with Reference Labs
- Prevent Double Billing
- Maintain Accurate Records
Consult with a Qualified Lab Billing Consultant
Medical billing regulations for laboratories are complex and constantly changing. Partner with lab billing consultant to ensure your lab stays up-to-date and avoids leading to pass-through billing.
The best thing? We offer a revenue and billing consultation session at no charge to you, so you can decide accordingly.
Don’t Contract Out In-House Tests and Bill as Your Own
It might be convenient to contract with an independent lab to perform tests you do in-house and then bill for them as your own. But this is a classic example of pass-through billing and a clear violation of regulations.
Stay Informed About Exceptions
The exceptions for pass-through billing are extremely limited and complex. You require strict adherence to specific criteria. Consult with us for lab billing services to avoid any violation.
Establish Written Agreements with Reference Labs
If your lab uses reference labs for legitimate testing needs, establish clear written agreements outlining the roles and responsibilities of each party. These agreements must specify billing procedures and ensure both labs understand their obligations.
Prevent Double Billing
Double billing is a major risk with pass-through billing for labs and practices. Put internal controls in place to ensure your lab doesn’t submit claims for tests already billed by the reference lab. At LBS, we conduct regular audits and reconciliation processes to help you identify potential discrepancies.
Maintain Accurate Records
Maintain clear documentation for all tests, including those referred to reference labs. The documentation must include details like test type, reference lab used, and any applicable modifiers.
Key Takeaway by LBS
Understanding pass-through billing is important for labs and physicians. In most cases, you must avoid it because it’s generally illegal. However, when outsourcing a test from another lab, you must implement proper billing procedures.
To avoid pass-through billing violations and maintain compliance, consider using our medical billing services, which are specialized for laboratories in the US.
