Independent healthcare providers, private practices, and multi-location hospitals can ensure timely reimbursement for laboratory services by staying updated with the recent lab billing and coding guidelines.
This Lab Billing Services guide to laboratory billing and coding helps you learn the seamless billing process, best practices, future trends, essential tools, and the overview of proper CPT code ranges for laboratories, ensuring efficient claim processing to achieve your laboratory’s financial growth.
What is Lab Billing and Coding
Lab billing is a specialized process of how laboratories get reimbursed or paid for their services. It ensures that the tests and analyses performed in the lab translate into accurate charges (coding) and proper reimbursement from insurance companies on behalf of their associated patients.
At the heart of laboratory medical billing lies a standardized coding system called Current Procedural Terminology (CPT) codes. These unique alphanumeric codes represent specific laboratory services.
When a laboratory performs a test, the corresponding CPT code is assigned to it. This code is then used to create a bill that accurately shows the service rendered.
Key Players in Lab Billing and Coding
While laboratories perform the tests, players like providers, lab staff, lab billing team, and payers are also involved in the billing process.
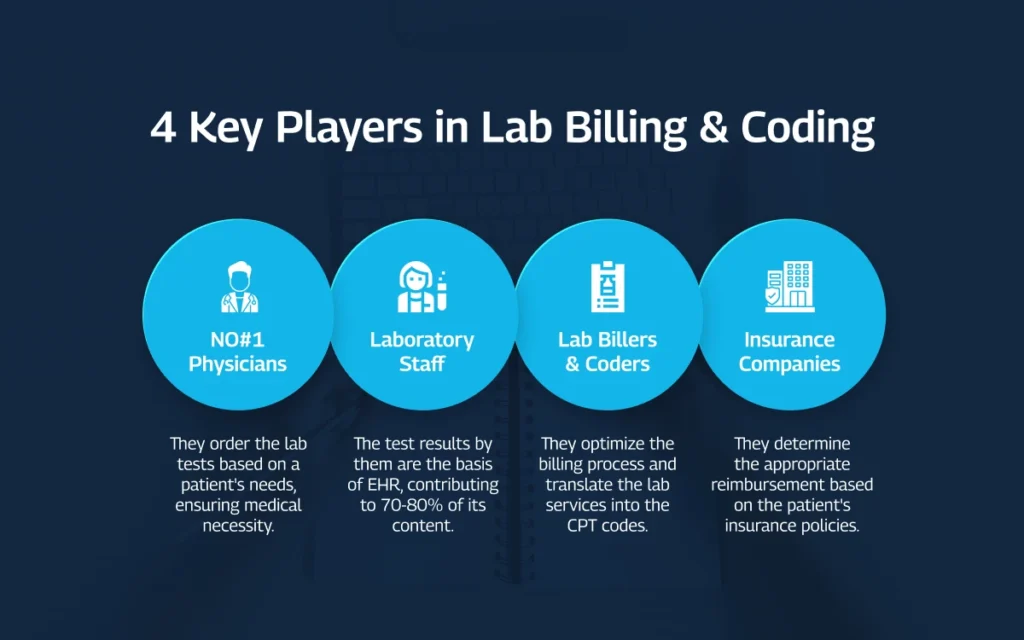
Physicians order the laboratory tests based on a patient’s needs, ensuring medical necessity for the tests being performed.
Laboratory staff perform the tests, ensuring accurate results.While financial considerations are important, laboratory testing plays a crucial role in patient care. The results of these tests are also the basis of EHR, contributing to 70-80% of its content.
Lab billers and coders optimize the billing process and translate the laboratory services into the appropriate CPT codes for labs.
Insurance companies receive the claims submitted by the laboratory and determine the appropriate reimbursement based on the lab CPT codes and the patient’s insurance coverage policies.
Why Care for Lab Billing and Coding Guidelines
Laboratory billing and coding are extremely important for:
- Accurate lab reimbursement
- Clear communication between labs and other key players
- Accurate collection of valuable healthcare data for improved patient care.
And that’s not just it!
Accurate and efficient billing practices ensure continued access to these vital diagnostic services. The complexities of laboratory testing calls for a specialized approach to billing. That is why growth-focused labs outsource their medical billing and coding operations to Lab Billing Services.
With our lab-specific lab billing expertise and experience to ensure efficient and accurate claim submission, we help maximize reimbursement for your laboratory so your lab technicians can focus on high-quality testing and accurate results.
Laboratory Billing Process
Understanding the lab billing process is extremely important to ensure properly implemented laboratory billing guidelines. The multi-step journey helps accurate claim submission, maximizes reimbursement, and keeps your finances healthy.
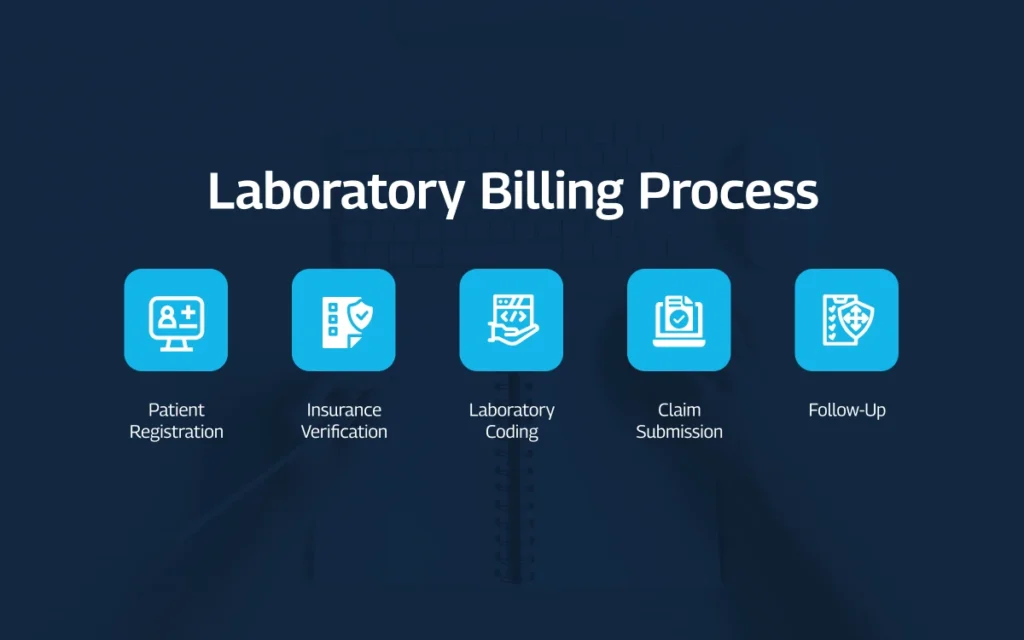
1 Patient Registration
The first step involves collecting demographic information such as the patient’s name, date of birth, address, and contact details. Also, the laboratory gathers insurance information, including the patient’s insurance provider, policy number, and any relevant group IDs. Accurate patient registration is the bedrock for successful claim processing.
2 Insurance Verification
During insurance verification, we confirm whether the specific laboratory services being ordered are covered under the patient’s insurance plan. Verifying coverage helps avoid unpleasant surprises for patients and ensures the lab bills the appropriate entity, the insurance company or the patient directly.
3 Assigning the Right Lab Codes
After the lab test is performed and analyzed, a skilled coder steps in to append the correct medical codes and modifiers to it. These codes are based on standardized coding systems like HCPCS and CPT. Incorrect or incomplete coding leads to claim denials, payment delays, and lost revenue for the laboratory.
4 Claim Submission
With the correct lab codes in place, a claim is generated. This electronic document essentially details the services provided to the patient, the associated codes, and the amount being billed. We, as a lab billing company, submitted the claim electronically to the insurance company for processing and reimbursement.
5 Follow-Up
Even after carefully following the laboratory billing and coding guidelines, your lab claims may be denied. In such cases, the laboratory’s billing team follows up with the insurance company to understand the reason for denial and work towards resolving the issue, ensuring timely and accurate reimbursement.
Note: Medical laboratory billing process is a collaborative effort between various healthcare players we discussed earlier in this guide. We ensure clear communication between all the parties involved to ensure the rightful reimbursement for your laboratory services. Contact us for a free lab billing audit right now.
7 Best Practices to Ensure Proper Laboratory Billing Guidelines
Smooth financial management is important for labs to thrive in the ever-changing healthcare landscape. It also ensures robust revenue cycle management for labs. Let us share7 key strategies to optimize accuracy, efficiency, and maximize reimbursement.
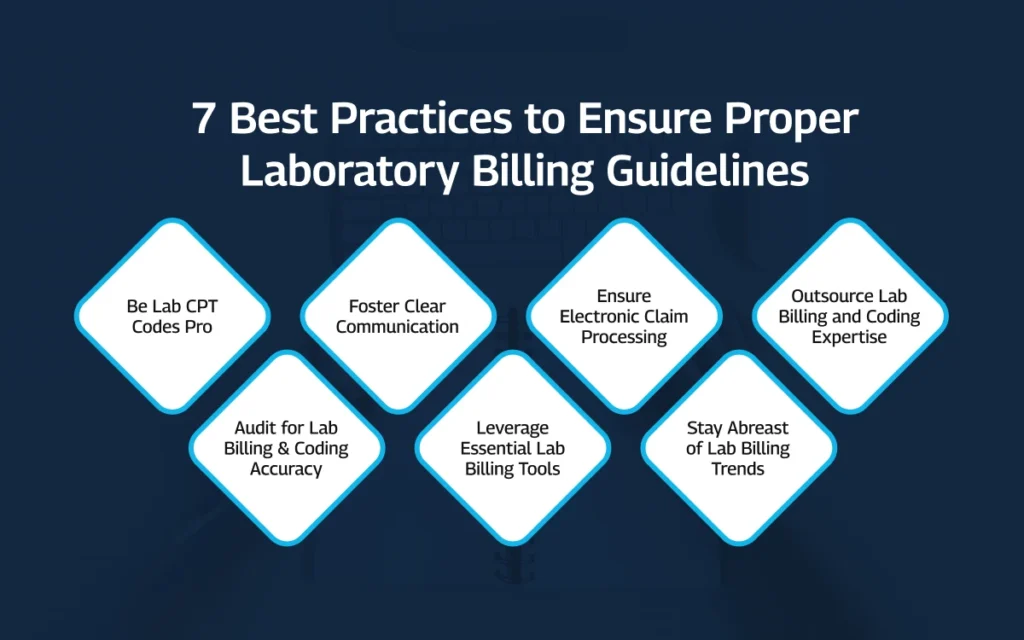
1. Be a Lab CPT Codes Pro
Laboratory procedure codes act as a universal language for defining the specific laboratory tests and procedures performed. Understanding the Current Procedural Terminology (CPT) coding ensures financial stability and streamlined operations.
CPT codes are alphanumeric identifiers typically containing five digits. The American Medical Association (AMA) publishes and maintains the entire CPT code set, with specific ranges designated for various laboratory procedures.
Let us share some commonly used CPT code ranges for labs.
80047-89356: Chemistry Procedures
This range consists of tests used to evaluate a patient’s metabolic state and organ function. The examples for this code range are cholesterol, glucose, liver function tests, and kidney function tests.
85025-85027: Complete Blood Count (CBC) Procedures
These CPT lab codes cover procedures related to CBC analysis, offering detailed information about the cellular components of the blood. This includes red blood cell (RBC) count, white blood cell (WBC) count, and differential WBC count.
86000-86063: Blood Coagulation Procedures
Essential for assessing a patient’s bleeding risk, these lab CPT codes represent tests related to blood clotting function, for example, prothrombin time (PT) and thrombin time.
87040-87899: Microbiology Procedures
87040-87899: Microbiology Procedures code range covers tests used to detect and identify various microorganisms such as bacteria, viruses, and fungi. These tests include cultures, sensitivity testing, and nucleic acid amplification tests.
81000-81003: Urinalysis Procedures
Urinalysis procedural codes showcase tests performed on urine samples to assess kidney function and detect potential abnormalities, involving both dipstick analysis and microscopic examination.
82000-84999: Pathology and Laboratory Procedures
These laboratory procedure codes cover many laboratory procedures beyond the categories mentioned above. And it includes lab services like tissue examinations, immunopathology testing, and molecular pathology testing.
Let’s give you some specific examples to help you understand how CPT codes reflect precise laboratory services.
- 80048: Basic Metabolic Panel represents a single test that measures multiple blood analytes, including electrolytes, glucose, and kidney function markers.
- 85025: Complete Blood Count, Automated signifies an automated analysis of a blood sample, sharing various blood cell types and their quantities.
- 87045: Culture, Bacterial; Blood code shows a lab test where a blood sample is cultured to identify any present bacteria.
These examples may offer just the basic understanding of CPT codes for laboratory billing. But to become a lab CPT codes pro, you must refer to authoritative resources like CPT Codebook, Centers for Medicare and Medicaid Services, AAPC, AMA, AHIMA and our Lab Billing blog of course.
The landscape of laboratory billing and coding is constantly evolving. New codes are introduced, regulations are updated, and staying informed is paramount. And you must also invest in training programs for your billing and coding staff.
2. Audit for Lab Billing and Coding Accuracy
Regular audits, both internal and external, helps maintain a healthy billing and coding system for labs.
Internal audits conducted by a qualified member of your team can identify coding errors, inconsistencies in documentation, and potential areas for improvement. External audits, performed by a third-party agency, offer an objective perspective and ensure compliance with regulatory standards.
Let us take this opportunity to offer you a free billing and coding audit to minimize claim denials and lost revenue for your laboratory.
3. Foster Clear Communication
Clear communication between various healthcare key players directly impacts laboratory billing accuracy. You must establish regular communication channels to bridge the gap.
Coders rely on accurate documentation to assign the correct codes. Encourage physicians who order laboratory tests to provide clear and concise documentation of the medical necessity for each test.
The billing team interacts with patients and insurance companies to ensure patients understand financial implications of lab testing and facilitates smooth claim processing with insurance companies.
4. Leverage Essential Lab Billing Tools
Whether you manage lab billing and coding in-house or outsource solutions, you must leverage the right tools to optimize revenue and maximize reimbursement. Let us share some 4 important lab billing tools and software to optimize your revenue cycle.
1 Laboratory Information System (LIS)
A robust Laboratory (Management) Information System (LIS) serves as the central hub for your laboratory’s data. It doesn’t just simply store test results and patient information but also enhances your billing practices by offering these functionalities:
- Identify the causes for delays and inefficiencies in the revenue cycle.
- Provide valuable insights into future performance and challenges.
- Ensure your lab stays compliant with ever-evolving medical billing and coding regulations with features like automated code validation and updates reminders.
2 Instant Adjudication Tools
With instant adjudication tools integrated into your lab billing workflow, you don’t need to wait for claim submission. Let us share what good adjudication tools can do for you.
- Verify a patient’s insurance coverage in real-time with no delays.
- Instantly file lab claims electronically and receive an immediate response from the insurance company for faster claim processing and quicker reimbursement.
3 ICD-10 Converter Software
ICD-10 coding systems can be complex, especially for smaller laboratories. This is where ICD-10 converter software comes in handy.
These are some of the top benefits of such software solutions:
- Code lab services quickly and accurately.
- Convert legacy lab codes to the current ICD-10 coding standards.
4 Laboratory Billing Software
Comprehensive laboratory billing software offers a suite of features beyond basic claim submission, including automated coding assistance, denial management tools, and reporting capabilities.
5 EHR Integration
Integrating your laboratory billing system with your EHR allows for seamless data transfer without manual data entry, reducing errors and improving efficiency.
5. Ensure Electronic Claim Processing
Manual claim submission is a recipe for errors and delays in laboratory billing and coding. Investing in robust lab billing software helps optimize your RCM process.
These are a few benefits of software solutions offering electronic submission of claims.
Automated Data Entry
Reduce the risk of human error by automating data entry tasks, such as capturing patient demographics and insurance information.
Code Lookup and Selection
Utilize the software’s built-in code lookup features to ensure accurate code selection based on the services rendered.
Lab Claim Scrubbing
Many software programs offer claim scrubbing functionalities that identify potential errors before claim submission, preventing delays and denials.
Streamlined Workflow
Laboratory billing software streamlines the overall workflow, allowing your team to focus on core competencies and improve overall profitability.
6. Stay Abreast of Lab Billing Trends
Staying abreast of healthcare billing and coding trends is crucial for laboratories to maintain efficient operations.
a) AI and ML
Artificial intelligence and machine learning are rapidly changing the way laboratory billing and coding work. These tech can offer these benefits to optimize your lab billing and coding processes.
- Analyze large medical data to identify coding inconsistencies.
- Suggest the most accurate codes for specific services.
- Predict potential claim denials and identify improvement areas.
- Frees up valuable time for coders to focus on complex cases.
- Automate repetitive tasks such as data entry, code selection, and claim scrubbing, reducing the risk of human error.
- Monitor regulatory updates and ensure the laboratory billing guidelines are compliant with changing standards.
b) Telemedicine
As telemedicine services become more prevalent, new codes and billing practices will emerge to reflect these changes. Staying updated on the evolving billing guidelines for laboratories is challenging.
These are just a few of the most common challenges to adapting telemedicine.
- Using data collected through telemedicine consultations in lab billing and coding operations to ensure accurate documentation.
- Making clear communication channels between telemedicine providers, laboratories, and patients will be essential for accurate service ordering, billing, and claim processing.
c) Value-Based Care
The healthcare industry is shifting from traditional fee-for-service models to value-based care models. Under these trending models, healthcare providers are reimbursed based on patient health outcomes rather than the volume of services performed.
These are our predictions for value-based care and reimbursements for labs:
- Medical lab coding will be more detailed, showing the services and the care quality.
- Detailed data analysis will become increasingly important to show the value labs bring to the patients and justify reimbursement under value-based models.
Embracing these emerging trends can help laboratories adapt to future laboratory billing guidelines and coding practices.
7. Outsource Lab Billing and Coding Expertise
Outsourcing your laboratory billing and coding needs to Lab Billing Services is a cost-effective solution, especially for small labs or those with limited in-house billing resources. It also frees up valuable time and resources within the laboratory, allowing you to focus on your core competencies like providing high-quality diagnostic services.
Our experienced lab coders and billing specialists are up-to-date on the latest regulations and lab billing and coding guidelines. Contact us right now for free consultation so you can decide wisely and accordingly.

