Medical laboratories are now under more payer scrutiny than ever. Aetna, in particular, enforces strict rules. Its stance on pass-through billing changes how labs bill and how they stay profitable. If ignored, these policies can severely impact your revenue.
Understanding Aetna lab pass-through billing policy can help your lab avoid thousands of dollars in denied claims. It can also make your billing workflow more efficient. This guide explains Aetna’s pass-through billing rules, exceptions, and compliance strategies.
You’ll find clear steps for clean claim submission to reduce pass-through billing errors and avoid delays. It’s important for labs that work with multiple referring providers or serve out-of-network patients. Let us help your lab from unnecessary denials and audits.
What is Lab Pass-Through Billing Policy of Aetna?
Aetna’s lab pass-through billing policy prohibits providers from billing for laboratory services that they did not perform. Only the lab that actually runs the test can submit the claim to Aetna. The ordering provider or referring physician cannot submit the bill, even if they collect the specimen or coordinate the process.
Aetna reimburses based on the CLIA (Clinical Laboratory Improvement Amendments) certification of the provider performing the service. This applies to both in-network and out-of-network situations. It doesn’t matter who ordered the test.
What matters is who did the test.
This rule helps Aetna ensure transparency in its payment processes. It cuts out middle layers and limits the potential for fraud or inflated markups. Aetna only wants to pay the lab that delivered the service. This also allows better tracking of outcomes and provider quality.
What Is Pass-Through Billing and Why It Matters to Labs?
Pass-through billing happens when one provider bills for services done by another. In labs, this usually means a physician’s office sends a sample to an outside lab. But instead of letting that lab bill, the office bills the insurer.
Here’s a quick example:
Dr. Smith collects blood from a patient. The samples are sent to a regional lab. Dr. Smith’s office then bills Aetna, pretending it did the test. This inflates costs. It hides who actually performed the work. It also leads to confusion and compliance issues.
Pass-through billing can also delay payment. If Aetna finds out the claim came from the wrong provider, it will be denied. That puts strain on your cash flow. Worse, it could flag your lab for an audit.
Aetna Lab Pass-Through Billing Policy Explained
Aetna will deny claims if the billing provider is not the testing lab. This rule applies across the board. It includes physicians, outpatient centers, and even other labs acting as billing intermediaries.
The test-performing lab must submit the claim directly. No middle billing allowed. Aetna enforces this rule using the National Provider Identifier (NPI). The NPI on the claim must match the lab that ran the test.
If there’s a mismatch, the claim will be denied. It doesn’t matter if the test was necessary. It doesn’t matter if there was prior authorization.
Aetna’s goal is a clean audit trail. It wants to see a direct line between the billed service and the provider that did the work. This allows them to verify credentials, check for fraud, and control costs.
Exceptions to Aetna Lab Pass-Through Billing Policy
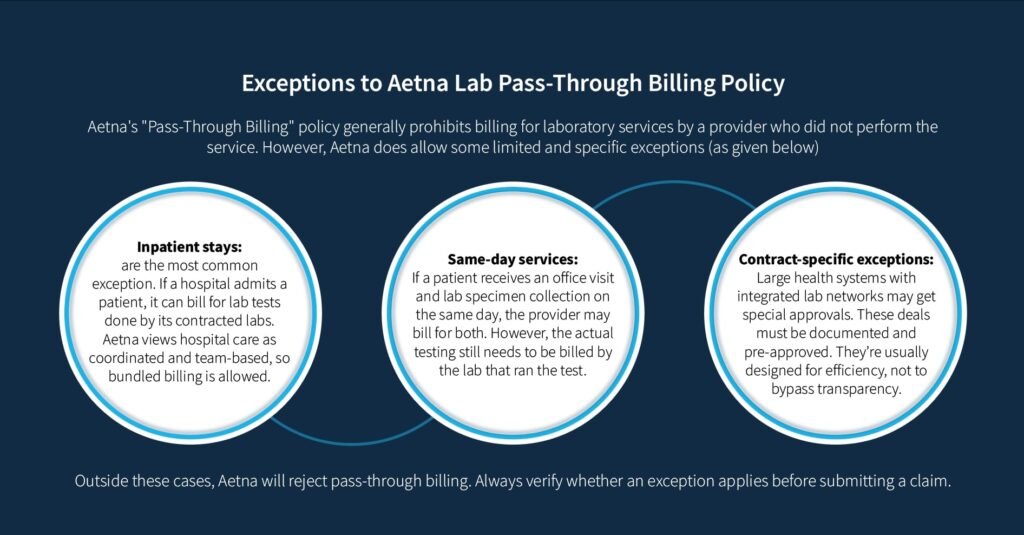
Aetna does allow some exceptions, but they are limited and specific.
Inpatient stays are the most common exception. If a hospital admits a patient, it can bill for lab tests done by its contracted labs. Aetna views hospital care as coordinated and team-based, so bundled billing is allowed.
Another exception applies to same-day services. If a patient receives an office visit and lab specimen collection on the same day, the provider may bill for both. However, the actual testing still needs to be billed by the lab that ran the test.
Some contract-specific exceptions also exist. Large health systems with integrated lab networks may get special approvals. These deals must be documented and pre-approved. They’re usually designed for efficiency, not to bypass transparency.
Outside these cases, Aetna will reject pass-through billing. Always verify whether an exception applies before submitting a claim.
Why Aetna and Other Payers Restrict It?
Payers are cracking down on pass-through billing because of fraud and cost inflation. When a third party bills for lab work, it opens the door to inflated pricing, billing mistakes, and even false claims.
Aetna’s policy protects its members. It prevents overbilling and ensures accurate reimbursement. It also makes it easier to track which providers are meeting quality and compliance standards. This helps eliminate confusion, reduces administrative layers, and improves claims accuracy. It also reduces risk for both the payer and the performing lab.
CLIA Certification and Its Role in Reimbursement
Every lab billing Aetna must have an active CLIA certificate. The certification must match the complexity of the tests being performed.
There are three levels for tests complexity:
- Waived
- Moderate complexity
- High complexity
Medical labs performing complex tests must have higher-level CLIA credentials. Aetna cross-checks the CLIA certificate with each billed CPT code.
If the code requires high-complexity certification and your CLIA is only moderate, the claim is denied. Even if everything else is correct, the mismatch will trigger a denial.
Aetna may also review CLIA compliance and look for outdated or invalid certifications. If your lab’s CLIA status lapses, claims will stop being paid. In some cases, Aetna may end your contract entirely.
What to Do: Stay current. Always update your CLIA number with payers. Run internal audits regularly to catch mismatches early.
What This Means for Medical Labs
Aetna lab pass-through billing policy means these things for labs:
- Ensure detailed documentation and claim submission
- Labs must bill Aetna directly
- Collaborate carefully with referring providers
- Watch for common lab billing errors
- Evolve with Aetna’s pass-through billing guidelines
1. Ensure Detailed Documentation and Claim Submission
Your CLIA number must be on every claim. It must match the complexity of the test. Documentation must clearly show this link.
Claims must also match the proper test codes to your certification level. If your lab handles both waived and high-complexity tests, double-check that each is correctly assigned. Mismatches lead to denials and lost revenue.
2. Labs Must Bill Aetna Directly
Do not rely on referring providers to bill Aetna. Set up direct billing systems. Make sure your lab is in-network where possible. This gives you better rates and faster claims turnaround.
Use billing software that handles payer rules. Automate where you can to cut down on manual errors. Always verify eligibility and benefits before testing.
3. Collaborate Carefully with Referring Providers
Referring practices need to know Aetna’s rules too. Educate them to avoid duplicate billing or confusion. Create agreements that define who handles what. Share protocols for specimen handling, insurance verification, and result reporting. Good communication reduces mistakes and ensures clean claims.
4. Watch for Common Lab Billing Errors
The most common reason for denials is listing the wrong NPI. Make sure your lab’s NPI is listed as the billing provider. Also check your place of service codes. They must reflect where the test was done, not where the specimen was collected.
Check your CLIA info for errors or outdated data. Even a single wrong digit can trigger a denial. Perform regular claim audits and use denial trends to fix issues early.
5. Evolve with Aetna’s Pass-Through Billing Guidelines
Policies change. Aetna updates billing rules often. Always review provider bulletins, newsletters, and manual revisions. Join lab associations or industry groups. They often track payer policy updates. Make sure your staff is trained regularly on new billing protocols.
Note: Adapting early helps you avoid costly delays or rejected claims.
How a Medical Billing Partner Can Help Your Laboratory
A good medical billing partner stays current with payer policies. They watch for changes and help you stay compliant. They also help reduce your denial rate and improve cash flow.
Lab billing is specialized. It involves unique codes, CLIA rules, and payer requirements. General billing services may miss key details. A lab-specific billing partner like Lab Billing Services (LBS) understands your workflows and your risks.
We, at LBS, can also provide ongoing training and support. Our team of lab billing specialists track denied claims, identify trends, and help implement corrections quickly. This lets your team stay focused on lab operations, not paperwork.
FAQs for Aetna Lab Pass-Through Billing Policy
What is pass-through billing for labs?
Pass-through billing occurs when a healthcare provider bills insurance for laboratory tests performed by another facility. The ordering provider receives test results from an external lab but bills patients or insurers as if they performed the testing in-house.
Is pass-through billing illegal?
Yes, in some cases. Pass-through billing violates federal healthcare laws like the False Claims Act, Stark Law, or Anti-Kickback Statute. It becomes illegal especially when tied to financial incentives or influences billing practices.
What is Aetna’s mutually exclusive policy?
Aetna’s mutually exclusive policy prevents billing for services that can’t reasonably be performed together. It’s due to anatomical, temporal, or gender-related factors. Based on CMS guidelines, this policy eliminates duplicate billing for inherently linked or incompatible procedures. For example, procedures that conflict by body part or timing.
Can a provider bill Aetna on our behalf if we perform the test?
Yes, in-network providers can bill Aetna directly for tests you perform under certain cases. Out-of-network providers require prior authorization. And Aetna may cover services at in-network rates when approved. However, the performing laboratory must be properly identified in billing documentation.
What lab settings qualify for exceptions?
These lab settings qualify for exceptions in lab pass-through billing:
- Inpatient hospital services
- Same-day specimen collection with office visits
- Forensic testing for legal cases
- Public health or research testing with no diagnostic purpose
- Some direct-to-consumer test kits
