No, you cannot bill 80307 and G0480 them together on the same day for the same patient.
Here’s why:
On July 1, 2023, CMS (Centers for Medicare & Medicaid Services) introduced a new rule. They added an NCCI edit that prevents billing 80307 (presumptive drug test) and G0480 (definitive drug test) together for the same patient on the same date of service.
Even if both tests are medically necessary, CMS will not pay for both when performed on the same day. One of the codes will be denied no matter what.
So what should you do? If both tests are required, perform the presumptive test first and then the definitive test on a different day. Always make sure to document clearly why both tests were necessary.
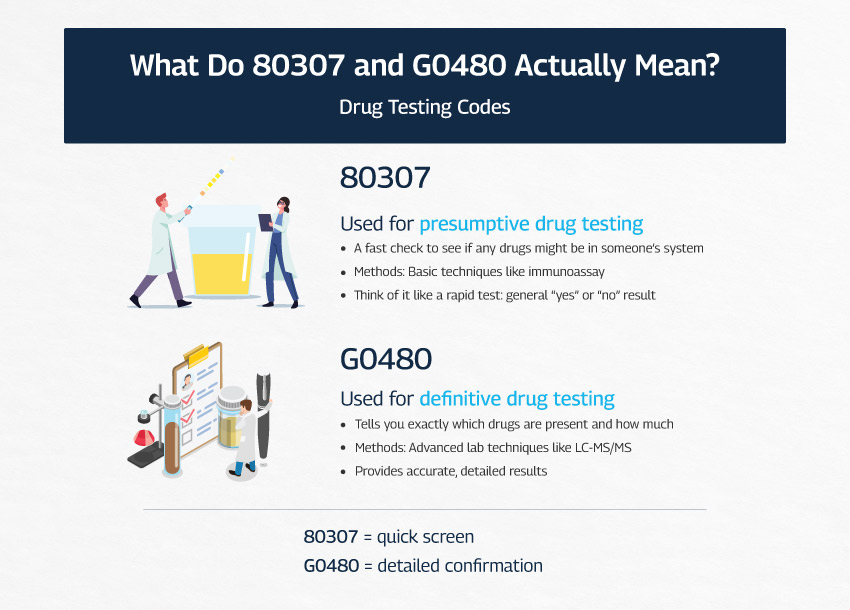
What Do 80307 and G0480 Actually Mean?
Let’s keep it simple.
80307 = quick screening
80307 is a presumptive drug test. It is a quick screen that checks whether drugs might be present. Labs typically run it on automated immunoassay or chemistry analyzers. Think of it as a rapid check that gives a general yes or no, without details.
G0480 = detailed confirmation
G0480 is a definitive drug test. It is the deep dive, usually performed with LC-MS/MS (liquid chromatography mass spectrometry). Instead of just indicating presence, it identifies the specific drugs and provides much more precise information.
You usually start with 80307 to get an overall idea. If the screen is unclear or raises concerns, you follow up with G0480 to get specific answers. However, remember that CMS does not allow both tests to be billed on the same day for the same patient, so timing matters.
Why You Cannot Bill Both 80307 and G0480?
There are several reasons why CMS made this rule, and understanding them can help you avoid denials and compliance issues.
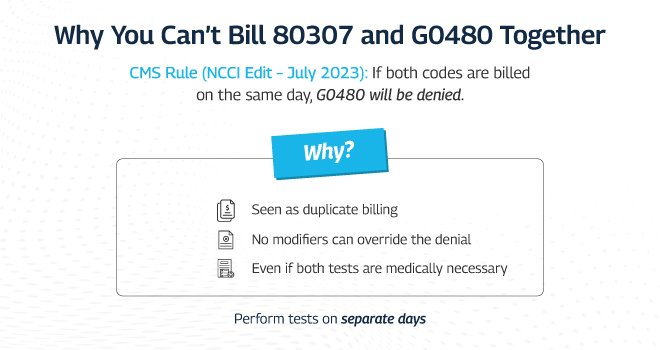
1). They answer the same clinical question on the same day
80307 is a quick screen. G0480 is a detailed confirmation. When both are billed for the same patient on the same date of service, Medicare views that as testing the same thing twice. That looks like duplicate billing, even if your clinical intent was good.
2). CMS put a hard stop in place
As of July 1, 2023, CMS added an NCCI edit that pairs these two codes as mutually exclusive for the same patient on the same date. If both appear on the claim, G0480 is automatically denied.
This is because CMS saw overuse and possible abuse of billing both codes together. By making the system deny G0480 automatically, they eliminated the gray area and forced providers to separate the services.
3). It is a compliance and cash flow risk
Submitting both codes together can trigger denials, slow down payments, invite audits, and create potential compliance issues. Even if you believe both were medically necessary, the claim will not be paid for both.
This is because Medicare wants healthcare providers to follow the “stepwise” approach: first do the quick screen, then if needed, order the definitive test on a different day. If you ignore this rule, your practice risks lost revenue, repeated denials, and even red flags from auditors who monitor billing patterns.
4). Modifiers do not fix it
Currently, modifiers such as 59 or XU cannot bypass the NCCI edit between 80307 and G0480. Here’s why:
- Some code pairs are flagged as “no-modifier allowed”
CMS assigns each NCCI Procedure-to-Procedure (PTP) edit a Correct Coding Modifier Indicator (CCMI). A CCMI of “0” means no modifier can override the billing restriction, while a CCMI of “1” means modifiers may be used in certain approved situations. For 80307 and G0480, CMS set CCMI = 0, so it’s a hard rule that modifiers can’t override the denial.
- CMS wants to stop these services from being billed together, period
The logic is simple: CMS deemed that doing both tests on the same day for the same patient is unnecessary and opens the door to abuse. They intentionally made the rule unbypassable to prevent misuse (even if a modifier is added).
- Modifiers only work when clinical circumstances clearly separate services
In other instances—for example, procedures on different body parts or separate visits—modifiers can justify billing both. But here, since both tests are typically done in sequence for the same clinical purpose, modifiers don’t apply.
Are 80307 and G0480 Ever Allowed on the Same Day?
Yes, there are exceptions, but they are not automatic and depend on timing and local policies. On October 1, 2023, CMS removed the national NCCI edit that had blocked billing 80307 and G0480 together on the same date of service. This change was made retroactive to July 1, 2023. That means the automatic hard stop is no longer in place, and claims are now processed under the regular coverage and payment rules. However, this does not mean you can freely bill both codes together for every patient.
Payment decisions now fall under the authority of your local Medicare Administrative Contractor. Each MAC has its own Local Coverage Determinations that spell out when presumptive and definitive tests are considered reasonable, how often they can be performed, and what documentation is required. If you decide that both tests are truly needed on the same day, your records must make that necessity clear. You should state why the screen alone was not sufficient, and why the definitive test was also essential for that specific patient encounter.
In practice, this means you should always check your MAC’s LCD, follow its guidelines closely, and document thoroughly before billing both tests together. Even though the NCCI edit is gone, CMS still expects strong justification. In short, you may be able to bill 80307 and G0480 together, but only if your MAC allows it and your documentation fully supports the medical necessity.
A Practical Guide to Billing 80307 and G0480
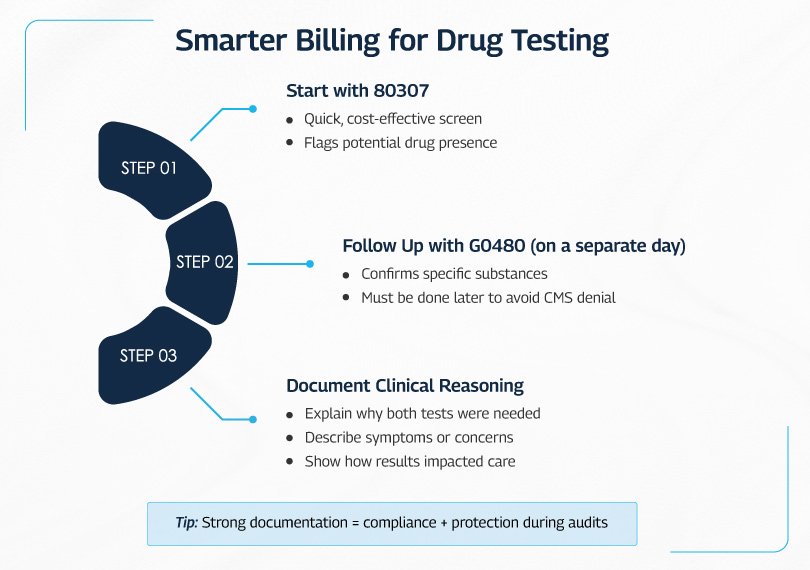
When you bill for drug tests like 80307 (presumptive) and G0480 (definitive), the process matters as much as the codes. Follow this approach to stay compliant and avoid denials.
Step 1. Start with the presumptive test (80307)
Use the quick screen first. It is fast, cost effective, and shows whether drugs might be present. Think of it as a red flag detector. It points you to a concern but does not provide full detail.
Step 2. Follow with the definitive test (G0480) only when justified
Order the definitive test when the screen is unexpected, unclear, or clinically concerning. Check your MAC policy before billing both on the same date.
- If your MAC allows same day billing in specific situations, document the medical necessity clearly and follow any frequency or diagnosis rules.
- If your MAC does not allow same day billing, perform and bill G0480 on a different date of service.
Step 3. Document the clinical reasoning
Strong notes are essential. Make it obvious why you needed both tests for this patient.
- Explain why both were needed. The screen did not answer the clinical question or showed something unusual, so you ordered a more specific test to confirm.
- Describe the concern. Note symptoms, behaviors, medication history, risk of overdose, adherence issues, or conflicting prescriptions. Be specific.
- Show how results affected care. Link the findings to actions such as medication changes, tapering, referral, safety planning, or further evaluation.
Good documentation does more than check a box. It protects you during audits, supports medical necessity, and aligns your claim with payer policies.
Conclusion
In summary, use 80307 for the initial screen and order G0480 for confirmation only when it is truly necessary. CMS no longer has a blanket ban on billing both on the same day, but your local MAC decides if it is allowed. Always review your MAC’s rules, document clearly why both tests were needed, and show how the results guided patient care, or you risk denials.
Lab Billing Service That Handles Drug Testing Codes the Right Way
Billing for lab tests especially drug screens like 80307 and G0480 isn’t just about plugging in codes. It takes real know-how to get it right.
At Lab Billing Services, we have coders who rely on expertise, not assumptions. They know when a presumptive test should be billed, when a definitive test is allowed, and how CMS edits affect each claim. They’ve worked through the NCCI restrictions, MAC policies, and the documentation that backs it all up.
